This white paper is the third of three parts on the complex functions of brain, what happens when an injury is acquired and how to care for and manage a life-changing brain injury.
BY LINDA SIMMONS, RN BScN
Consultant and Cost of Future Care Expert, Connect Medical Legal Experts
The prehospital care of a patient with a brain injury has a profound impact on the subsequent course of events and outcomes. Prehospital management refers to the initial resuscitation and interventions that stabilize the patient at the scene of the accident and on route to the hospital. Prehospital management requires timely and effective brain resuscitation, as the brain only has minimal reserves to meet ongoing metabolic needs. If resuscitation is insufficient because of reduced cerebral blood flow (CBF) and decreased oxygen delivery, ischemia and hypoxia develop and can lead to secondary brain injury.
Many of the patients who have a Traumatic Brain Injury (TBI) also suffer other life threatening injuries. Advanced Trauma Life Support (ATLS) is a set of standards that has been developed to prepare health care professionals in the effective management of trauma victims. Trained personal are taught to quickly triage and stabilize the patient. Primary and secondary survey is used when assessing the trauma victim. A brief description of primary and secondary survey is presented, and a more in depth discussion of TBI management follows.
Primary Survey
Primary survey includes airway, breathing, circulation, and disability (ABCD’s). Airway patency must be secured, having the patient speak is a quick way to confirm an adequate airway, however, the patient that has blood, or foreign material in the oropharynx must be removed by suction or manually. A patient who is obtunded (e.g. Head injury, shock, intoxication) requires intubation to assist in airway patency.
Breathing can be compromised in TBI and especially in serious motor vehicle accidents. Head injury, shock, and intoxication can cause a decreased central respiratory drive. Injuries to the chest (hemothorax, pneumothorax, rib fractures, and pulmonary contusion) can also compromise breathing. Auscultation of the chest, and inspection for tracheal deviation and subcutaneous air can determine chest injuries. Intubation may be required to ensure adequate ventilation, and the insertion of a chest tube to remove blood and/or air from the pleural space.
Circulation can be compromised by apparent hemorrhage; however internal hemorrhage is less obvious. Internal hemorrhage can occur in the chest, abdomen, pelvis or thigh (pelvic or femur fracture). Blood pressure (BP) and pulse (P), and signs of shock (dusky colour, diaphoresis, altered mental status) are assessed. The abdomen is assessed for distention and tenderness, and the thigh is assessed for deformity and instability, pelvic instability is assessed. External bleeding is controlled by direct pressure. It is important to initiate an intravenous with Ringer’s lactate or 0.9% Normal Saline to prevent hypovolemic shock.
Hypotension and tachycardia are usually a result of injury other than the head injury. Hypotension often indicates there is bleeding located elsewhere (abdominal, pelvic, or thoracic cavity). Hypotension in a person with a brain injury decreases Cerebral Blood Flow (CBF) and Cerebral Perfusion Pressure (CPP) (the difference between mean arterial pressure (MAP) and intracranial pressure [ICP]).
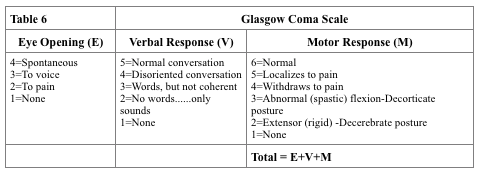
Disability is the final stage of the primary survey. Neurological function to determine brain and spinal cord injury is completed. The Glascow Coma Scale (see below) for adults and the modified GCS for infants and children and pupillary response will determine brain injury. Sensation and gross motor movement will determine if there has been a spinal cord injury. The patient is immobilized on a fracture board and cervical collar is applied to stabilize the neck.
Secondary Survey
The secondary survey is completed once the patient is stable. At this time, a history is obtained. The acronym used to get a quick history with only the essential information is “AMPLE”: Allergies, Medications, Past medical history, Last meal, and Events of the injury. The examination of the patient generally is done using a head to toe assessment. Inspection include inspection of the skin for swelling, lesions and any obvious deformities, palpation of bones for tenderness, and range of motion to assess joints.
The seriously injured patient and the obtunded patient will usually have a urinary catheter inserted and a nasogastric tube placed. These procedures are contraindicated if there is evidence of urethral injury or if there is the presence of midface trauma. Open wounds are covered with sterile dressing. Dislocations or marked deformities that are causing neurovascular compromise are reduced immediately. Other obvious or suspected fractures can be splinted.
Testing is completed for the injured patient. X-rays are the most necessary test when determining extent of the patient’s injuries. The areas to be x-rayed are varied. Chest, cervical spine, and pelvic x-rays are the first to be completed. Cat scan and ultrasound are frequently used to assess abdominal injuries and for more definitive exam of other injuries. Head CT is obtained for patients with altered mental status and for those who have had loss of consciousness.
Other x-rays may be obtained for suspected fractures. Laboratory tests include Arterial Blood Gases (ABG’s), urinalysis, Complete Blood Count (CBC). Other blood tests may be required if the patient’s medical history warrants it (e.g. electrolytes, coagulation studies, blood alcohol and drug screens). Those patients who have had a significant blunt trauma to the chest require an Electrocardiogram (ECG) to diagnose cardiac injury.
Traumatic Brain Injury-In-Hospital Care
Clinical severity of head injury is frequently assessed using the Glascow Coma Scale, pupillary size and response (PERRLA-pupils equal, round, reactive to light and accommodation), and motor function (lateralization suggest focal lesion).
The Glascow Coma Scale (Table 6, right) is the most widely used assessment tool for level of consciousness. A GCS score of 13 or higher indicates a possible mild brain injury; 9 to 12 is a moderate injury and 8 or less a severe brain injury. In the Statutory Accident Benefits Schedule a catastrophic impairment is a GCS score of 9 or less. The proper way of charting the GCS score requires documentation of each component, therefore documenting a GCS 9 is not sufficient, it should be documented E3V3M3 = GCS 9.
There are limitations using the GCS for patients who have been intubated or sedated, paralysis, facial swelling, hypotension, hypoxia, alcohol or illicit drug intoxication. These patients may not be able to provide responses in all the categories of the GCS. In these situations, a 1 is given with an additional comment for example for eye opening it would be E1c where c= closed, and for verbal response it would be V1t where t=intubated. GCS 5tc is an example of a documented score; the patient’s eyes are closed due to swelling equaling a 1, and the patient is intubated equaling a 1 and motor score would then be a 3 for abnormal flexion.
Secondary injury can occur if the patient with TBI does not have adequate ventilation, oxygen and brain perfusion. Therefore, management is aggressive to prevent hypoxia, hypercapnia, hypotension, and increased ICP. As mentioned previously, internal and external bleeding need to be rapidly controlled, and fluid replacement is essential (crystalloids, blood transfusions) to maintain cerebral perfusion.
Mild injuries (Table 6) occur in about 80% of patients who have TBI and require treatment. Typically, they have had a brief loss of consciousness (LOC) or no LOC. They have stable vital signs, normal CT scan and normal neurologic function. These patients are usually discharged home to the care of a family member who will observe them for an additional 24 hours. The observer is instructed to return to the hospital if the patient experiences decreased LOC, focal neurological deficits, worsening headache, vomiting or deterioration of mental function.
Patients who have had brief LOC and abnormal or mental neurologic function are often observed overnight and follow-up CT is done in 4-8 hrs. If a patient has minor abnormalities on hents who have had brief LOC and abnormal or mental neurologic function are often observed overnight and follow-up CT is done in 4-8 hrs. If a patient has minor abnormalities on head CT they may need a follow up CT in 24 hours. If the 2nd CT is normal and neurologic status is stable these patients can be discharged.
Twenty percent of brain injuries are considered moderate or severe. Patients who have suffered a moderate head injury (Table 6) have LOC between 1 to 24 hours, and a period of post-traumatic amnesia of up to 24 hours. They do not usually require intubation and mechanical ventilation (unless other injuries are present) or ICP monitoring. These patients require admission and observation regardless of whether their CT is normal.
Severe TBI are admitted to a critical care unit. These patients are intubated due to impaired protective reflexes. Preventing and controlling ICP is critical, if ICP remains high further cerebral damage can occur. Patients requiring intubation and mechanical ventilation are intubated using Rapid Sequence Intubation, this method of intubation uses sequential administration of pre-determined doses of a hypnotic drug and a rapid-acting neuromuscular blocker. This method of intubation prevents coughing and gagging and minimizes risk of an increasing ICP.
Neurosurgical consultation is required once the patient has been stabilized. The CT findings will determine whether the patient will need surgical evacuation. CT can identify subdural hematomas, subarachnoid hemorrhage, intracerebral hematomas, infarcts, diffuse brain injury, and cerebral edema. Evacuation is done immediately if a subdural or epidural hematoma is greater than 5 mm in thickness, and there is a midline shift. Surgical repair (craniotomy/craniectomy) is also required if there is evidence of a depressed, open or compound skull fractures and assisting in reducing ICP.
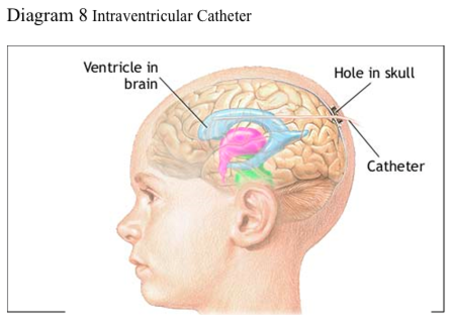
ICP monitoring is integral in the management of patients with severe head injuries. Methods vary in monitoring ICP; however, intraventricular catheters (catheter threaded into one of the lateral ventricles of the brain) are preferred. These catheters provide continuous measurement of ICP and allow drainage of CSF to control increased ICP. Diagram 9 illustrates the positioning of an intraventricular catheter. Mannitol boluses are used to decrease ICP when other methods have not been successful. Continuous infusions of mannitol (once a standard) can cause intravascular dehydration and hypotension.
Diagram 8 Intraventricular Catheter
Volume replacement is necessary to keep the brain profused and the goal is to maintain a mean arterial pressure of greater than 90 mm Hg (roughly the average of systolic and diastolic pressure).
Analgesia and sedation are required control negative (increased ICP and BP) responses to pain and noxious stimuli. Narcotics such as morphine or fentanyl are considered to be the most appropriate because they offer both analgesia and depression of airway reflexes. Propofol (short acting anaesthetic) is also used. It is titratable and when discontinued the effects ware off quickly. The advantage of propofol is it provides predictable sedation, and yet still allow for neurological assessments.
Hyperthermia requires aggressive treatment. It can be caused by infection, central injury to the hypothalamus, cerebral irritation from hemorrhage or drug response to anticonvulsants. Hyperthermia increase the cerebral metabolic rate and thus putting the patient at risk for inadequate oxygen supply at a cellular level and ultimately secondary injury. Identifying the cause and treating it aggressively is critical. Acetaminophen and cooling measures can be used. The goal is to maintain normal temperature while preventing shivering.
The patients head should be elevated to 30 degrees. This assists in the prevention of pneumonia. Seizures should be treated with anticonvulsants, to prevent any further brain injury.
In severe head injuries, there is an increased risk of gastric irritation, gastric ulcers, and gastrointestinal hemorrhage (Cushing’s ulcer). Prophylactic medications such as Zantac or Pepcid are given to prevent gastric complications. Bowel programs are instituted to prevent constipation. Early nutritional support assists in maintaining the integrity of the gastric mucosa, and has been shown to reduce risk of infection. Enteral nutrition either by nasogastric or gastronomy tube is recommended.
There are several preventative care needs required for the patient with TBI. When the patient is unconscious, their eyes often remain open. Facial injuries can cause irritation and abrasions to the eyes. It is imperative to protect the corneas by lubricating them with artificial tears and applying eye patches.
The unconscious patient is at risk for skin breakdown. Preventing skin breakdown includes using assistive devices to frequently reposition the patient. Meticulous skin care and application of skin barriers can prevent skin breakdown. Lastly, the use of special surfaces can reduce skin breakdown. The areas most at risk are bony prominences.
Contractures can occur because of the nature of the brain injury and with decreased activity. It is important to use methods that will maintain correct body positioning. Splints, pillows and passive range of motion exercises can prevent contractures.
Sensory stimulation is important for the unconscious patient. Health professionals and family members should touch and talk to the patient. Nurses can talk to the patient while they are providing care. It is important to try to maintain usual day and night patterns. Family members can participate with sensory stimulation by reading to the patient. Often having the favourite patient’s favourite radio channel or TV show can be excellent methods of stimulation. When the patient is arousing from a coma, they often become agitated. Although this is a good clinical sign, the agitation and confusion the patient exhibits can be distressful to family members. It is imperative during this time to attempt to decrease stimulation and allow the patient frequent rest periods.
Family members of the patient are integral in caring for the patient. Families go through stages of grieving (denial, anger, bargaining, depression, and acceptance). It is important to listen and allow the family to express concerns and feelings. Communication about the patient’s condition is necessary both to reinforce and clarify the myriad of information that may be occurring. Allowing the family to participate in caring for the patient is beneficial for both the patient and the family. The Rancho Levels of Cognitive Functioning (1990) is a tool that describes behavioural characteristics and cognitive deficits associated with brain injury. As the patient progresses and their behaviours and cognitive deficits change, this tool is helpful to the health care team, and to family members. It provides understanding of what is happening to the patient and focuses on the patient’s disabilities (see Appendix A). Supporting family in decision-making re: post-hospitalization management and placement is crucial when choices about care options are required.
The management of patients with severe head injury is complex and requires a multidisciplinary approach. The ultimate goal is to prevent further secondary injury. The management discussed in this document provides an overview of the initial care for patients suffering TBI.
GLOSSARY
Agnosia – loss of ability to recognize objects, persons, sounds, shapes, or smells while the specific sense is not defective nor is there any significant memory loss
Anterograde amnesia – loss of ability to form new memories, although older memories may be safe (good memory of the years before the injury, but relatively little memory for anything that happened since)
Aphasia – loss of the ability to produce and/or comprehend language, due to injury to brain areas specialized for these functions. Depending on the area and extent of the damage, someone suffering from aphasia may be able to speak but not write, or vice versa, or display any of a wide variety of other deficiencies in language comprehension and production, such as being able to sing but not speak. Aphasia may co-occur with speech disorders such as dysarthria or apraxia of speech.
Apraxia – loss of the ability to execute or carry out learned purposeful movements, despite having the desire to and the physical ability to perform the movements
Ataxic (ataxia) – gross in-coordination of muscle movements
Broca’s asphasia – language is reduced to disjointed words and sentence construction is poor
Comminuted Skull Fracture – skull splintered or shattered into pieces
Depressed Skull Fracture – fragment of the skull is depressed with or without tearing of dura mater [three layers of the meninges surrounding the brain and spinal cord]
Dysarthria – is a speech disorder that is due to a weakness or in-coordination of the speech muscles. Speech is slow, weak, imprecise, or uncoordinated.
Dystonia – involuntary contractions of muscles resulting in twisting and repetitive movements. Sometimes they are painful.
Diffuse visual field defects – overall blurred vision
Emotionally Labile – refers to the pathological expression of laughter, crying or smiling
Linear Skull Fracture – single fracture line
Multiple field loss – areas of darkness that appear to be scattered around objects
Open Depressed Skull Fracture – opening of the skull as a result of comminuted depressed skull fracture and tearing of the dura mater and the scalp
Pseudodepression – condition following a massive lesion in the frontal lobe of the brain, characterized by apathy, indifference, and loss of initiative but no experience of depression
Pseudopsychopathic – characterized emotional and social instability, aggressive behaviour (at times), cognitive disturbances described as a special form of incoherence, abnormal social behaviour in the form of social adhesiveness, carelessness, and a certain proneness to criminality
Tunnel vision (constriction) – objects in the center of the visual field are visible, but those on the edges are not
Visual Field Cuts – complete or partial loss of peripheral vision. People with visual field loss may have problems seeing objects out of the corner(s) of their eyes, losing their place while reading, being startled by people or objects moving toward them, or bumping into people and objects.
References
Evidence-Based Review of Moderate to Severe Acquired Brain Injury (ERABI) (2006). Retrieve March 24, 2008 from http://www.abiebr.com/index_home.html
Centre for Neuro Skills TBI Resource Guide (2006). The brain map. Retrieved March 3, 2008 from http://www.neuroskills.com/brain.shtml
Deitch, E. A., & Dayal, S. D. (2006). Intensive care unit management of the trauma patient. Critical Care Medicine, 34 (9), 2294-2301.
Discovering Psychology (2008). The human brain. Retrieved on March 3, 2008 from http://www.learner.org/discoveringpsychology/brain/brain_flash.html.
Fakhry, S. M., Trask, A. L., Waller, M. A., & Watts, D. D. (2004, March). Management of brain-injured patients by an evidence-based medicine protocol improves outcomes and decreases hospital charges. The Journal of Trauma Injury, Infection and Critical Care, 56(3), 493-500.
Granacher, R. P. (2005). Traumatic brain injury: Methods for clinical and forensic neuropsychiatric assessment. Boca Raton, Florida: CRC Press.
Hebb, M. O., Clarke, D. B., & Tallon, J. M. (2007, June). Development of provincial guideline for the acute assessment and management of adult and pediatric patients with head injuries. Canadian Journal of Surgery, 50 (3), 187-194. Retrieved February 26, 2008, from http://www.cma.ca/index.cfm/ci_id/52773/la_id/1.htm
Karol, R. L. (2003). Neurpsychosocial intervention: The practical treatment of sever behavioural dyscontrol after acquired brain injury. Boca Raton, Florida: CRC Press.
Marik, P. E., Varon, J., & Trask, T. (2002, August). Management of head trauma. Chest, 122(2), 699-711. Retrieved February 22, 2008, from http://chestjournal.org/cgi/content/abstract/122/2/699
Ministry of Health Promotion (2007). Ontario’s injury prevention strategy: Working to together for a safer, healthier Ontario. Retrieved February 20, 2008, from http://www.mhp.gov.on.ca/english/injury_prevention.pdf
National Institute of Neurological Disorders and Stroke (2002). Traumatic brain injury: Hope through research. Retrieved February 21, 2008, from http://www.ninds.nih.gov/disorders/tbi/detail_tbi.htm
The Merck Manuals Online Medical Manual (2007). Retrieved March 1, 2008, from http://www.merck.com/mmpe/sec21/ch310/ch310a.html
Nolan, S. (2005, April-June 2005). Traumatic brain injury: A review. Critical Care Nursing Quarterly, 28(2), 188-194.
The Brain Injury Recovery Network (2003). Injury overview. Retrieved February 20, 2008, from http://www.tbirecovery.org/overview.html
The Rancho Levels of Cognitive Functioning (1990).Family guide to the rancho levels of cognitive functioning. Retrieved February 20, 2008 from http://www.rancho.org/patient_education/bi_cognition.pdf
Zoellner, J. L. (2003). Craniocerebral trauma. In J. V. Hickey (Ed.), Clinical practice of neurological & neurosurgical nursing (5th ed., pp. 373-403). Philadelphia, PA: Lippincott Williams & Wilkins.

