This white paper is the second of three parts on the complex functions of brain, what happens when an injury is acquired and how to care for and manage a life-changing brain injury.
BY LINDA SIMMONS, RN BScN
Consultant and Cost of Future Care Expert, Connect Medical Legal Experts
TBI refers to any injury to the scalp, skull (cranium or facial bones) or the brain. Injury to the brain can be focal or diffuse. Focal injuries result in contusions, lacerations, or hemorrhages. The hemorrhages that can occur are epidural hematoma, subdural hematoma, intracerebral hematoma, and subarachnoid hemorrhage. The diffuse injury can cause a mild to severe concussion or diffuse axonal injury.
Primary Brain Injury
Primary brain injury occurs one of two ways: contact phenomena or head motions acceleration and deceleration. Primary brain injury is the result of direct mechanical damage that occurs at the time of the trauma. These mechanisms are known as the coup and contrecoup mechanisms and causes superficial or contusional hemorrhage. 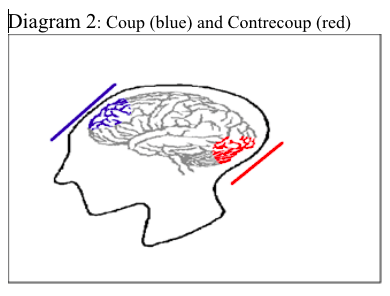
Coup injuries are caused when the head is stopped suddenly and the brain moves forward rapidly and strikes the side of the skull and the skulls inner ridges. Contrecoup injuries is caused when the brain bounces off the primary surface and then strikes the opposite side of the skull, this causes additional injury to the brain.
Diagram 2, right, shows both coup (blue) and contrecoup (red) mechanism of injury.
Acceleration and deceleration occurs when the different layers of the brain move at different times because each layer has a different density. This results in stress and strain being placed on the neurons and the axons that run though the brain. The axons can end up being stretched, sheared, twisted, or compressed. Blood vessels often are torn causing microscopic hemorrhage.
Injuries that occur at the time of the primary injury include injury to the scalp, skull fractures, meningeal tears, and traumatic brain injury. Traumatic Brain Injury is broken down into focal or diffuse injuries. Focal injuries include contusion, lacerations, and intracranial hemorrhages. Diffuse injuries consist of concussions and diffuse axonal injuries.
Scalp Injuries
The extent of scalp injuries depends on the velocity and characteristic of the impacting contact object. Injuries to the scalp are classified as abrasions, contusions, lacerations, and subgaleal hematoma.
Skull Fractures
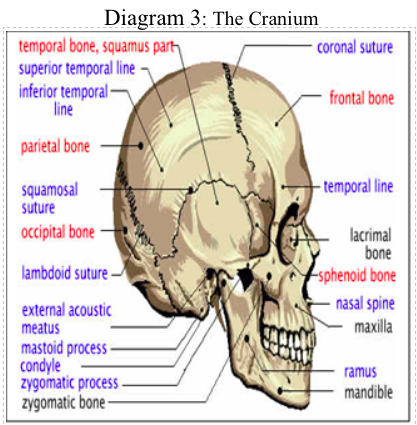
The skull consists of the cranium and the facial bones. The cranium (Diagram 3) houses the brain and is composed of the frontal, parietal, temporal, occipital, sphenoid, and ethmoid bones. The facial bones are the bones that provide a framework for our face. The facial bones include the maxillary, zygomatic, nasal, and lacrimal and mandible (only movable bone) bones. Facial bone fractures often occur in motor vehicle accidents (MVA).
The Cranium (Diagram 3)
The mechanism of skull injury is through direct contact. The factors that affect the degree of injury are the weight, velocity, and angle of the impact and the skulls thickness at the point of impact. The fractures that may occur are linear, comminuted, depressed and the scalp, open depressed fracture, and basal skull fracture (base of the skull is fractured and can be linear or depressed).
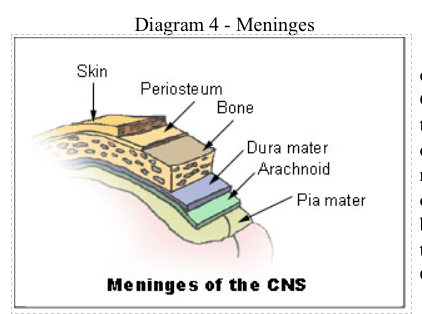
Basal skull fractures are more serious than fractures affecting other parts of the cranium. These fractures often cross over the air sinuses of the frontal bone or the air sinuses of the temporal bone. The bones in this area are fragile and adhere to the dura mater, and the consequence is leakage of cerebrospinal fluid (CSF) via a dura tear. Diagram 4, below right, provides the layers of the meninges.
The drainage of CSF from the nose is called rhinorrhea, and when the drainage of CSF is from the ear, it is known as otorrhea. In the emergency setting litmus paper is used to determine a CSF leak. The drainage from the nose or ear is usually bloody.
When the drainage is put on litmus paper, the blood will be encircled by a yellowish stain, and is called the “halo sign”. Other tests include testing the CSF drainage for glucose.
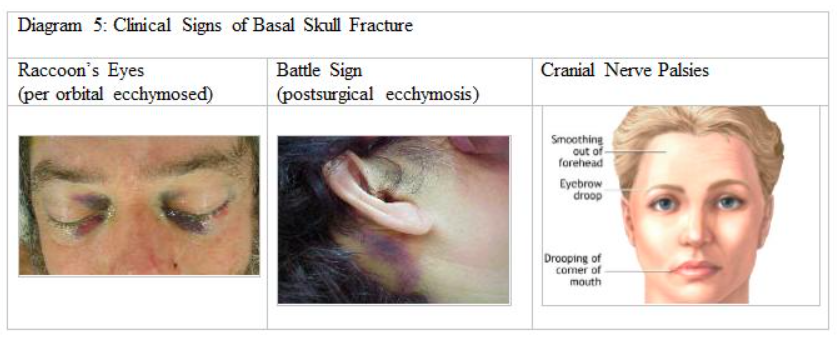
Clinically the patient often presents with postsurgical ecchymosed (Battle sign), bruising behind the ear; per orbital ecchymosed (raccoon eyes), bruising around the eyes; hemtympanum (presence of fresh blood within the middle ear gives the tympanic membrane a red or purple colour) and possible cranial nerve palsies (paralysis of the facial nerve).
Diagram 5 provides pictures of three of the four classic signs of basal skull fractures: Clinical Signs of Basal Skull Fracture Raccoon’s Eyes(per orbital ecchymosed) Battle Sign (postsurgical ecchymosis) Cranial Nerve Palsies, Raccoon Eyes (2) and Battle Signs.
Meningeal Tears
Tears in the dura mater can occur with basal skull fractures, depressed fractures in the temporal or frontal bones and with some facial fractures. As discussed previously, when the dura is torn, CSF leakage may occur from the ear, nose, or post nasally, and often blood is noted behind the tympanic membrane of the ear (hemtympanum).
Focal Brain Injuries
Contusions and Lacerations
Contusions (bruising) occur on the surface of the brain and can occur from blunt trauma (coup [directly under the area of impact] and contrecoup [opposite side of direct impact] injuries), depressed skull fracture, a penetrating wound, or an acceleration-deceleration closed injury. The movement of the brain within the skull identifies the location of the contusion.
The frontal and temporal areas of the cortex of the brain are most susceptible due to the ridges and irregularities at the base of the skull. The clinical impact of a contusion depends on its size and related cerebral edema (swelling). Smaller contusions may be asymptomatic; however, larger contusions may result in attention, emotional and memory deficits.
Cerebral edema can cause intracranial pressure (ICP) and herniation of the brain.
A cerebral laceration occurs when the tissue of the brain is mechanically cut or torn. Lacerations require greater physical force to cause injury than contusions. Lacerations occur in the same areas as contusions. In diffuse axonal injury, the corpus callosum (longitudinal fissure that connects the left and right cerebral hemispheres) and the brain stem are common locations for lacerations.
Hematomas
Intracranial hemorrhage is a common complication of TBI. Bleeding may begin immediately after the injury; however, its presence may not be apparent until a sufficient amount of blood accumulates to cause signs and symptoms. The time between bleeding and the appearance of clinical symptoms can range from minutes to weeks, depending on the site and rate of bleeding.
Some patients with mild TBI intracranial hemorrhage may be occult and there will be no loss of consciousness, while in other patients with hemorrhage unconsciousness may occur on impact. The major types of bleeding in TBI are epidural hematomas, subdural hematomas, and intracerebral hemorrhage.
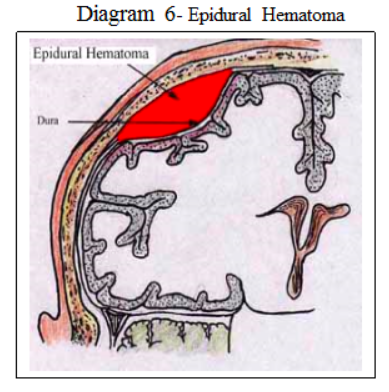
Epidural Hematoma
Epidural hematomas (EDH) are ovoid in shape and located outside the dura but within the skull, they are relatively uncommon. Epidural hematomas (Diagram 6) are arterial in origin and usually result from a tear of the middle meningeal artery in a patient who has suffered a skull fracture to the thin temporal bone. Most often, they are located in the temporal or temporal parietal region. EDHs are seen most often in children and young people.
Clinically the patient may have a momentary unconsciousness followed by a lucid period lasting minutes to several hours. This lucid period is followed by rapid deterioration from drowsiness, lethargy, and coma. The sequela is headache, seizures, hemiparesis or hemiplegia, posturing (decortication and decerebration), late signs are bradycardia and respiratory distress. Pupils show ipislateral (affected side) dilatation, sluggish and fixed responses to light. People with epidural hematoma are commonly referred to as patients who “talk and die” because they usually have a lucid phase followed by rapid deterioration. The overall mortality rate ranges from 9% to 33%. Operative decompression is the standard treatment.
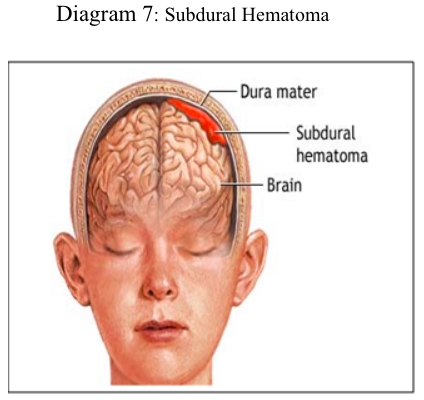
Subdural Hematoma
Subdural hematoma (SDH) refers to bleeding between the dura mater and the brain (Diagram 7). On CT scan SDH is crescent-shaped in appearance. SDH are more common than EDH and occurs in about 30% of severe head injuries. The mechanism of injury is due to tearing of the bridging vein that is located over the convexity of the brain. SDH is classified by the interval between the injury and the appearance of signs and symptoms. The three classification are acute (up to 48 hours), subacute (2 days to 2-3 weeks) and chronic (3 weeks to several months). SDH are also classified according to whether the blood is clotted (acute), mixed with clots and blood fluid (sub-acute) and blood fluid only (chronic).
Signs and symptoms of an acute SDH include gradual or rapid deterioration of level of consciousness (drowsiness to slow cerebration, to confusion and finally coma), papillary changes, and hemiparesis or hemiplegia. Subacute SDH present similarly to acute SDH. The patient who does not regain consciousness should be worked up for an SDH.
Patients who have had a “minor” TBI can develop symptoms months after the initial injury, and often they may not recall the initial injury. Repeated small bleeding occurs, and the SDH becomes apparent when the hematoma compromises the brain. It usually starts with a headache that increases in severity and progresses to symptoms similar to an acute or subacute SDH.
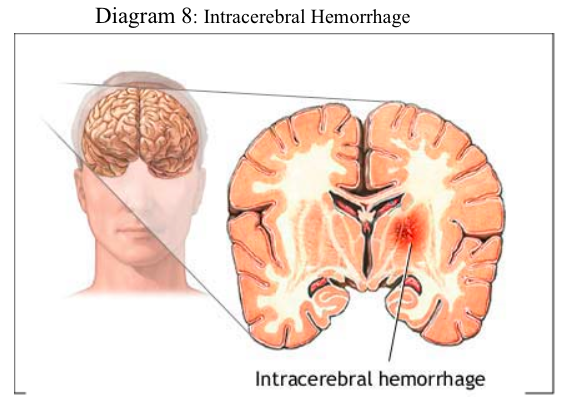
Intracerebral Hemorrhage
Intracerebral hemorrhage (ICH) can occur in all severities of head injuries. An intracerebral hemorrhage (Diagram 8) is bleeding in the brain caused by the rupture of a blood vessel. Clinically ICH appears as expanding, space occupying lesions. ICH usually occurs in the frontal and temporal lobes. At the time of the injury, the sudden rotation of the head cause the brain to strike or glide across the rough surface of the skull. Increased intracranial pressure (ICP) a nd clinical deterioration are the most common signs and symptoms.
Diffuse Brain Injury
Concussions
The word concussion means a violent shaking. Concussion may be caused by striking something or impulsive forces where the head is thrown forward suddenly. Concussions can be classed as mild (temporary neurological dysfunction no loss of consciousness) or classic (temporary neurological dysfunction, unconsciousness and memory loss). Concussions are considered to be a mild traumatic brain injury.
The signs and symptoms of a concussion can be subtle and may not appear immediately. Symptoms can last for days, weeks or longer. The two most common concussion symptoms are confusion and amnesia. The amnesia, may or may not be preceded by a loss of consciousness, but almost always involves the loss of memory of the impact that caused the concussion.
Other symptoms include, headache, dizziness, ringing in the ears (tinnitus), nausea and vomiting, and slurred speech. Other symptoms that may occur later include mood and cognitive disturbances, sensitivity to light and noise, and sleep disturbances. It is difficult to diagnose a concussion in young children; some of the symptoms displayed may be listlessness, tiring easily, irritability, crankiness, change in eating or sleeping patterns, lack of interest in favourite toys, loss of balance, and unsteady walking.
Diagnosis is based on both physical and neurological exams, duration of unconsciousness (usually less than 30 minutes) and post-traumatic amnesia (PTA) of less than 24 hours, (PTA; usually less than 24 hours), and the Glasgow Coma Scale (scores of 13 to 15). Neuropsychological tests can be administered hours, days, or weeks after the injury, or at different times to determine whether there is a trend in the patient’s condition.
The assessing healthcare practitioner must consider screening for more serious injury when the patient has worsening of symptoms, such as headache, persistent vomiting, increasing disorientation or a deteriorating level of consciousness, seizures and unequal pupil size.
Patients with such symptoms, or who are at higher risk for a more serious brain injury, are given MRIs or CT scans to detect brain lesions and is observed closely. Post-concussive syndrome occurs in about 10% of people who have a concussion.
It is more common after a serious concussion than after a mild one. The main symptom is persistent headache for one to two weeks, lasting up to months after the injury. Symptoms usually are relieved with mild pain relievers such as acetaminophen (Tylenol) or ibuprofen (Motrin, Advil). Other symptoms may be dizziness, difficulty concentrating or difficulties reading.
Nausea and vomiting has also been reported. Post concussive syndrome usually goes away on its own.
Diffuse Axonal Injury
Diffuse axonal injury (DAI) refers to injury to the axons that are located throughout the brain. Axons are long thin fibers that extend across. As discussed earlier acceleration-deceleration occurs when the different layers of the brain move at different times because each layer has a different density. This results in stress being placed on the neurons and the axons that run though the brain. The axons can end up stretched, sheared, twisted, or compressed. Blood vessels often tear causing microscopic hemorrhage. DAI accounts for almost half of all brain injuries and one third of all deaths from TBI.
The injured axons undergo a series of changes, and cause a cascade of pathophysiological events. Initially it is difficult to see axonal injury, but during the first several days after the injury, damaged axons increase in numbers and change. Eventually the ends of the sheared axons retract into globoid shapes known as retraction balls (hallmark of DAI). Diffusion-weighted MRI can identify DAI.
Secondary Brain Injury
Secondary brain injury occurs after the initial trauma, and is produced by a number of events and changes which occur after the injury. Biochemical changes and a release of a variety of substances (excitatory amino acids glutamate, aspartate, cytokines, and free radicals) initiates a harmful sequence of ongoing cell membrane breakdown and ionic shifts resulting in more damage to the injured brain. These processes include intracranial hemorrhage, brain swelling (cerebral edema), increased intracranial pressure (ICP), and hypoxic (ischemic) brain damage and infection.
Further, secondary injury to the brain can result from a critical event, series of events or multisystem complications. It is important to remember that people who have suffered a brain injury most often have other injuries that compromise the patient’s stability. Secondary injuries contribute to poor outcomes for the patient. Episodes of hypoxemia, systemic hypotension, sustained increased ICP, respiratory complications, electrolyte imbalance, and infections can lead to further damage to the brain.
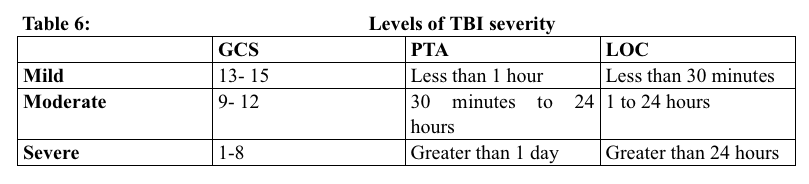
The severity of TBI can be categorized as mild, moderate, or severe and is useful in predicting outcome. A small number of patients may remain in a persistent vegetative state. These patients remain in a coma for months to years. Table 6 (bottom right image) uses GCS scale, and the duration of Post-Traumatic Amnesia (PTA) and Loss of Consciousness (LOC) to categorize severity of TBI.
Glossary of Terms
Agnosia – is a loss of ability to recognize objects, persons, sounds, shapes, or smells while the specific sense is not defective nor is there any significant memory loss
Anterograde amnesia – loss of ability to form new memories, although older memories may be safe (good memory of the years before the injury, but relatively little memory for anything that happened since)
Aphasia – loss of the ability to produce and/or comprehend language, due to injury to brain areas specialized for these functions. Depending on the area and extent of the damage, someone suffering from aphasia may be able to speak but not write, or vice versa, or display any of a wide variety of other deficiencies in language comprehension and production, such as being able to sing but not speak. Aphasia may co-occur with speech disorders such as dysarthria or apraxia of speech.
Apraxia – loss of the ability to execute or carry out learned purposeful movements, despite having the desire to and the physical ability to perform the movements
Ataxic (ataxia) – gross in-coordination of muscle movements
Broca’s asphasia – language is reduced to disjointed words and sentence construction is poor
Comminuted Skull Fracture – skull splintered or shattered into pieces
Depressed Skull Fracture – fragment of the skull is depressed with or without tearing of dura mater [three layers of the meninges surrounding the brain and spinal cord]
Dysarthria – is a speech disorder that is due to a weakness or in-coordination of the speech muscles. Speech is slow, weak, imprecise, or unco-ordinated.
Dystonia – involuntary contractions of muscles resulting in twisting and repetitive movements. Sometimes they are painful.
Diffuse visual field defects – overall blurred vision
Emotionally Labile – refers to the pathological expression of laughter, crying or smiling
Linear Skull Fracture – single fracture line
Multiple field loss – areas of darkness that appear to be scattered around objects
Open Depressed Skull Fracture – opening of the skull as a result of comminuted depressed skull fracture and tearing of the dura mater and the scalp
Pseudodepression – condition following a massive lesion in the frontal lobe of the brain, characterized by apathy, indifference, and loss of initiative but no experience of depression
Pseudopsychopathic – characterized emotional and social instability, aggressive behaviour (at times), cognitive disturbances described as a special form of incoherence, abnormal social behaviour in the form of social adhesiveness, carelessness, and a certain proneness to criminality
Tunnel vision (constriction) – objects in the centre of the visual field are visible, but those on the edges are not
Visual Field Cuts – complete or partial loss of peripheral vision. People with visual field loss may have problems seeing objects out of the corner(s) of their eyes, losing their place while reading, being startled by people or objects moving toward them, or bumping into people and objects.

